Post Time: 2025-07-18
Diabetes is a chronic health condition that affects how your body turns food into energy. It's characterized by elevated levels of blood glucose, or blood sugar, and can lead to serious health complications if not managed effectively. This comprehensive guide will walk you through everything you need to know about diabetes, from understanding the different types, to strategies for prevention and management, including lifestyle changes and medical treatments. This article aims to empower you with the knowledge needed to take control of your health and well-being.
Understanding the Different Types of Diabetes
Before delving into prevention and management, it's important to understand the various forms of diabetes. Each type has its own causes, mechanisms, and management requirements. Here’s a breakdown:
- Type 1 Diabetes: An autoimmune condition where the body's immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. People with type 1 diabetes need to take insulin daily for survival. This type is often diagnosed in childhood or adolescence, but it can occur at any age.
- Type 2 Diabetes: The most common type of diabetes, accounting for 90-95% of all cases. It occurs when the body becomes resistant to insulin or doesn't produce enough insulin to meet the body's needs. This type is often linked to lifestyle factors like obesity, inactivity, and poor diet, and can be managed effectively with lifestyle adjustments, oral medications, or sometimes insulin.
- Gestational Diabetes: Diabetes that develops during pregnancy, usually after the 24th week. It typically resolves after childbirth. However, women who have had gestational diabetes have a higher risk of developing type 2 diabetes later in life.
- Prediabetes: A condition where blood sugar levels are higher than normal but not yet high enough to be diagnosed as type 2 diabetes. Prediabetes is a critical stage, offering an opportunity to intervene and prevent the development of type 2 diabetes through lifestyle changes.
- Monogenic Diabetes Syndromes: Less common, caused by mutations in a single gene and affect specific biological functions, that are essential to managing diabetes. Examples include Neonatal diabetes and Maturity onset diabetes of the young (MODY).
| Type of Diabetes | Key Characteristics | Management |
|---|---|---|
| Type 1 | Autoimmune; Requires insulin injections for survival | Insulin therapy, diet, exercise, regular blood glucose monitoring. |
| Type 2 | Insulin resistance or deficiency; often linked to lifestyle factors | Lifestyle changes, oral medication, insulin therapy in some cases. |
| Gestational | Develops during pregnancy; resolves after childbirth; increases Type 2 risk | Careful diet planning, regular blood glucose monitoring, sometimes insulin. |
| Prediabetes | Blood glucose levels higher than normal, but not yet diabetic | Lifestyle changes focusing on healthy eating and regular physical activity. |
| Monogenic | Genetic conditions affecting insulin levels or actions | Highly individualized depending on condition |
Understanding the differences between these types is crucial for proper diagnosis, treatment, and overall management of diabetes. Each type may necessitate slightly different approaches and strategies for effective care.
The Importance of Early Detection and Diagnosis
Early detection of diabetes, especially type 2 and prediabetes, is crucial in preventing the progression of the disease and minimizing the long-term risk of complications. Many people with type 2 diabetes may have no noticeable symptoms initially, leading to delayed diagnosis and a potentially negative impact on long term health outcomes. Common symptoms that one may experience are:
- Increased Thirst: Feeling unusually thirsty even after drinking fluids.
- Frequent Urination: Need to urinate more often than normal, particularly at night.
- Unexplained Weight Loss: Losing weight without trying or due to increase loss of glucose.
- Increased Hunger: Experiencing excessive hunger, even after eating.
- Fatigue: Feeling tired or weak, not helped by rest.
- Blurred Vision: Vision becomes blurry or changes from the norm.
- Slow Healing Sores: Wounds or cuts take longer to heal.
- Frequent Infections: Prone to skin, vaginal or other frequent infections.
If you experience any of these symptoms, it is essential to consult a healthcare professional and undergo diagnostic tests.
Diagnostic Tests for Diabetes
The following tests are commonly used to diagnose diabetes or prediabetes:
- Fasting Plasma Glucose (FPG) Test: Measures blood sugar levels after an overnight fast (at least 8 hours of no food or caloric drinks). An FPG level of 126 mg/dL (7.0 mmol/L) or higher indicates diabetes; between 100 and 125 mg/dL (5.6 to 6.9 mmol/L) signifies prediabetes; and anything under 100 mg/dL (5.6 mmol/L) is normal.
- Oral Glucose Tolerance Test (OGTT): Measures blood sugar levels two hours after drinking a special sugar solution. A two-hour blood sugar level of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes; between 140 to 199 mg/dL (7.8 to 11.0 mmol/L) signifies prediabetes; and anything under 140 mg/dL is normal. This test is common during pregnancy to check for Gestational Diabetes.
- Random Plasma Glucose (RPG): Measures blood glucose levels at any time, regardless of meal history. Blood sugar levels at or above 200 mg/dL (11.1 mmol/L), along with symptoms, may indicate diabetes.
- A1C Test (Glycated Hemoglobin Test): Measures the average blood sugar levels over the past 2 to 3 months. An A1C level of 6.5% or higher indicates diabetes, between 5.7% and 6.4% signifies prediabetes and anything under 5.7% is normal.
Regular screening for diabetes is highly recommended, particularly for people who have risk factors such as a family history of diabetes, are overweight or obese, have high blood pressure or high cholesterol, are over the age of 45, have had Gestational diabetes and/ or have a family history of type 2 diabetes. Early diagnosis allows for timely intervention and significantly reduces the risk of developing complications associated with prolonged high blood sugar levels.
Proven Strategies for Diabetes Prevention
While Type 1 diabetes cannot be prevented due to its autoimmune nature, type 2 diabetes and gestational diabetes can be prevented or delayed through targeted lifestyle interventions. These strategies include:
1. Adopting a Healthy Diet
- Focus on whole foods: Prioritize consumption of foods that are in their most natural form such as fruits, vegetables, whole grains and lean proteins.
- Limit processed foods: Reduce your intake of processed foods, sugary drinks, and refined carbohydrates.
- Control portion sizes: Pay attention to your serving sizes and avoid overeating. Use smaller plates if required.
- Choose healthy fats: Replace saturated and trans fats with unsaturated fats like those found in nuts, seeds, and olive oil.
- Fiber intake: Increase consumption of dietary fiber through eating fruits, vegetables and whole grains which slows the absorption of sugar.
| Food Category | Recommended Choices | Foods to Limit |
|---|---|---|
| Fruits & Vegetables | Fresh, frozen, or canned with no added sugar | Fruit juice, canned fruits in syrup |
| Grains | Whole grains (brown rice, quinoa, oats) | White bread, white rice, refined pasta, pastries |
| Protein | Lean meat, poultry, fish, beans, lentils | Processed meats, fried foods |
| Dairy | Low-fat milk, yogurt, cheese | Full-fat dairy, sugary dairy drinks |
| Fats | Nuts, seeds, avocado, olive oil | Fried food, foods high in saturated fat |
2. Engaging in Regular Physical Activity
- Aim for at least 150 minutes of moderate-intensity exercise: Activities like brisk walking, swimming, cycling, or dancing will increase cardiovascular health.
- Incorporate strength training: Building muscle helps increase your metabolism and also increases glucose metabolism. Aim for at least two strength training sessions each week.
- Start gradually: If you're new to exercise, start slow and gradually increase the intensity and duration of your workouts.
- Make physical activity a routine: Find activities you enjoy and make them part of your daily life. Include your family members so it can be more enjoyable for everyone.
3. Achieving and Maintaining a Healthy Weight
- Weight loss: For overweight or obese individuals, even a modest weight loss of 5-10% can have a significant impact on reducing the risk of type 2 diabetes.
- Monitor your weight: Keep track of your weight and take steps to maintain a healthy body mass index (BMI).
- Adopt sustainable habits: Focus on long-term, sustainable changes to your eating and exercise habits, rather than quick fixes that you cannot keep up with.
- Balance calories and energy expenditure: To manage a healthy weight, balance the calories that you consume from foods with the amount of calories you burn through daily activity.
4. Managing Stress Levels
- Practice relaxation techniques: Engaging in relaxation practices such as yoga, meditation, or deep breathing exercises help reduce your overall stress levels.
- Ensure adequate sleep: Lack of sleep has been linked to an increase in blood glucose levels. Ensure that you have a regular sleep schedule and get adequate sleep.
- Take breaks when you need them: Ensure that your body has breaks during times of high stress. Take some time out for activities that bring you joy.
5. Regular Health Screenings
- Routine check-ups: Visit your physician regularly for routine medical check ups and request testing if any symptoms are present.
- Family history awareness: Be aware of your family health history of diabetes and other genetic risk factors and undergo early screening, if necessary.
- Monitoring: Maintain regular check-ups and engage in the various recommended screening methods.
By proactively adopting these preventative measures, individuals can reduce their risk of developing type 2 diabetes and significantly improve their overall health and wellness. It is essential to be consistent with any preventative or treatment steps.
Effective Strategies for Managing Diabetes
Managing diabetes effectively requires a comprehensive approach that integrates medical treatment with lifestyle changes. The goal of diabetes management is to maintain blood glucose levels within a healthy range, prevent long term complications and improve overall well-being. The following strategies are key in controlling blood sugar levels.
1. Blood Glucose Monitoring
- Regular checks: Monitoring blood glucose levels at home with a glucose meter is a core step in the effective management of diabetes, and you should use it to check before and after meals, exercise and when you are feeling unwell.
- Keep a log: Keep a log of your blood glucose readings, which you can share with your healthcare provider.
- Continuous Glucose Monitoring (CGM): CGM provides real-time blood glucose readings via a sensor that’s inserted under the skin, eliminating the need for frequent finger-pricks. CGM provides an accurate picture of how blood glucose levels change during the day and it provides a detailed log.
- Understand your target range: Work with your healthcare team to establish blood glucose target range that is appropriate for you. This range can be impacted by a number of factors including; age, activity, lifestyle etc.
| Monitoring Method | Frequency | Benefits |
|---|---|---|
| Home Glucose Meter | Multiple times daily (as directed) | Allows regular checks, helps manage medication and diet, relatively inexpensive |
| Continuous Glucose Monitor | Continuous readings throughout the day | Real-time insights, alerts, reduced need for finger-sticks, long-term data collection |
| A1C Test | Every 3-6 months | Provides an average of long-term blood glucose levels for an over view of management |
2. Medication and Insulin Therapy
- Oral medications: Several types of oral medications are available to help manage type 2 diabetes, each working differently to improve insulin sensitivity and regulate blood glucose levels. These need to be taken as directed by your healthcare provider, at specific intervals to ensure the best action from these medication.
- Insulin Therapy: Insulin is necessary for people with type 1 diabetes and may also be required for some individuals with type 2 diabetes or during pregnancy. It can be administered through injections or insulin pumps, under the direction of a healthcare provider.
- Working with your physician: Each person is different so a care plan, that works for you, will need to be customized by your health care provider. Ensure that you work closely with your healthcare team to ensure an optimal treatment regimen for your unique situation.
3. Consistent Meal Planning
- Work with a Registered Dietitian: This professional will be able to assist in creating individualized dietary plans specific to your individual nutritional needs.
- Consistent meal times: Regular meals with appropriate spacing throughout the day is essential to maintaining optimal blood sugar levels.
- Meal content: Choosing the right meals is essential for managing your blood glucose. Include balanced macro and micro nutrients to assist in reducing blood glucose levels.
- Portion sizes: Pay close attention to the portion sizes as this plays a vital role in controlling blood glucose levels.
- Glycemic index (GI): GI refers to how quickly foods impact your blood glucose. Select foods with a lower glycemic index so your blood glucose will stay more stable.
4. Regular Physical Activity
- Schedule activities: Include at least 150 mins per week of moderate physical exercise to reduce the blood glucose levels and increase insulin sensitivity.
- Regularity: Ensure that exercise is part of your regular routine and keep a consistent exercise plan to help stabilize your blood sugar.
- Consult health care provider: Check with your health care provider before starting any exercise routine.
- Types of exercises: Variety in your exercise is recommended and this could include cardio or strength training. Choose an exercise that you enjoy.
5. Lifestyle Management
- Stress Management: Practice relaxation exercises or other stress management practices to help reduce glucose levels that can increase with stress.
- Adequate Sleep: Ensure that you are getting the right amount of sleep to reduce your stress levels. Aim for at least 7-8 hours per day and consistent sleep times.
- Quit smoking: Smoking is one of the leading causes of various diseases and this applies to blood glucose. Smoking makes it harder to manage diabetes and may increase the overall risks.
- Regular Check Ups: It is important to keep regular appointments with your physician to monitor your treatment and medication plans to ensure the best care for you.
Effective diabetes management is a lifelong commitment that requires consistency, education, and support. Working closely with your healthcare team, along with adoption of effective lifestyle habits, helps manage your overall wellness. It is possible to live well with diabetes by staying vigilant and well educated about diabetes.
Managing the Long-Term Complications of Diabetes
Untreated or poorly managed diabetes can lead to a variety of severe health complications that affect almost all areas of the body. Long-term complications develop when your blood glucose levels remain high over a prolonged time. Being informed about potential long-term risks helps to mitigate some of these problems and assists with long-term management of overall health.
Here are some common complications and effective measures for addressing them:
1. Cardiovascular Disease
- Risk Factors: Uncontrolled high blood sugar levels can damage the blood vessels, increasing the risk of heart disease, strokes, and peripheral artery disease.
- Management: Effective control of blood sugar levels, along with managing blood pressure and cholesterol through diet, exercise, and sometimes medication, are very important.
2. Neuropathy (Nerve Damage)
- Impact: High glucose levels can damage the small nerves and blood vessels, resulting in pain, numbness, and tingling in the extremities, especially the hands and feet.
- Management: Careful monitoring of glucose levels, managing pain through appropriate treatments and proper foot care to prevent foot problems.
3. Nephropathy (Kidney Damage)
- Impact: Chronic high blood sugar levels may damage the kidneys, potentially leading to kidney failure.
- Management: Careful management of blood sugar and blood pressure, along with regular urine checks for protein and maintaining optimal kidney function are all essential to preventing and managing this disease.
4. Retinopathy (Eye Damage)
- Impact: High glucose levels can damage the blood vessels in the retina, leading to vision loss and blindness.
- Management: Routine eye exams, early detection of problems, and maintaining ideal glucose levels are all vital for minimizing long term retinal damage. Laser treatment and other advanced approaches are used to prevent further loss of sight.
5. Foot Problems
- Impact: Nerve damage and poor circulation increases the likelihood of developing foot ulcers, infections and issues with healing.
- Management: Practicing good foot care, regular checks, and timely intervention to address any issues to prevent further injury.
6. Skin Conditions
- Impact: Individuals with diabetes are prone to skin infections and other related issues, often including dry or itchy skin conditions.
- Management: Proper care of skin including keeping the area moisturized, clean, dry to prevent long-term conditions from developing.
| Complication | Symptoms | Prevention and Management |
|---|---|---|
| Cardiovascular | Chest pain, shortness of breath, leg pain, fatigue | Blood sugar, blood pressure, cholesterol control; heart healthy diet; regular exercise |
| Neuropathy | Numbness, tingling, pain in hands and feet | Blood sugar control; pain management; proper foot care |
| Nephropathy | Swelling, fatigue, change in urine amount | Blood sugar and blood pressure management; urine testing for protein |
| Retinopathy | Blurred vision, floaters, vision loss | Blood sugar control; regular eye exams; timely intervention |
| Foot Problems | Sores, ulcers, infections, numbness, pain | Blood sugar control; regular foot care; professional foot exams |
| Skin Conditions | Infections, dry skin, itching, blisters | Blood sugar control; hygiene; use of skin moisturizing products; medical intervention if required |
Prevention and early detection is essential in minimizing long-term complications associated with diabetes. Managing this chronic condition involves maintaining ideal blood glucose levels, regular checkups and proactive management of your overall health, wellness and dietary habits. Working closely with your medical provider, you can avoid most, if not all of the associated complications and live well with this condition.
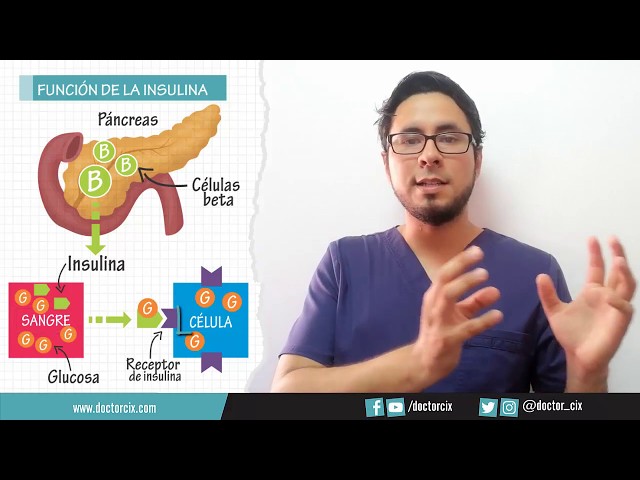
Aquí te explico cuál es la what is the normal blood sugar level for adults diferencia principal entre la does tomatoes raise blood sugar diabetes can coffee raise blood sugar mellitus tipo 1 y tipo 2