Post Time: 2025-07-18
Hypoglycemia, or low blood sugar, is a common and potentially dangerous complication for individuals with diabetes, especially those who also suffer from neuropathy. Understanding the nuances of hypoglycemia, particularly in the context of neuropathy, is critical for managing the condition effectively. This article will delve into the unique challenges and symptoms of low blood sugar for diabetics with neuropathy, emphasizing the importance of early recognition and proactive management. Diabetes, particularly when poorly managed, can cause nerve damage—diabetic neuropathy—affecting various parts of the body, including the peripheral nerves in the hands and feet, autonomic nerves affecting heart rate and digestion and even cranial nerves. This nerve damage can mask or alter the typical symptoms of low blood sugar, making it more difficult to detect and manage effectively. This presents a complex scenario that necessitates vigilance and a tailored approach.
Why is Hypoglycemia Dangerous for Those with Neuropathy? The core issue is that neuropathy can interfere with the body’s usual warning systems. Normally, when blood sugar levels drop too low, the body releases hormones like adrenaline, causing symptoms like shaking, sweating, and rapid heartbeat. However, neuropathy can blunt these responses. Specifically:
- Autonomic neuropathy, which affects the nerves controlling internal organs, can diminish the adrenal response that triggers these typical symptoms.
- Peripheral neuropathy, common in the extremities, may make it harder for a person to perceive the early warning signs, such as tingling, before a dangerous episode occurs.
These diminished reactions mean individuals may not feel the usual warning signs of hypoglycemia until it’s very severe, significantly increasing the risk of fainting, seizures, or other severe complications, including serious cognitive impairment. This altered experience with hypoglycemia leads to a state known as hypoglycemia unawareness, making effective management even more challenging. This condition is particularly concerning in Type 1 diabetics, where the risk of hypoglycemia is often higher due to reliance on exogenous insulin.
The Altered Landscape of Hypoglycemic Symptoms in Neuropathy
For those without neuropathy, the body typically provides several clear indications of low blood sugar levels. Common symptoms include shakiness, dizziness, sweating, increased heart rate, and hunger. However, individuals with neuropathy often experience these symptoms differently, or not at all. It's vital to know the specific ways hypoglycemia can present itself when nerve damage is present. The impact of neuropathy on the symptoms of hypoglycemia isn’t always straightforward and can vary from person to person. Here's a detailed breakdown:
Common Symptoms of Hypoglycemia in Non-Neuropathic Individuals:
| Symptom | Description |
|---|---|
| Shakiness | Trembling or feeling unsteady |
| Sweating | Perspiration that may be excessive |
| Rapid Heartbeat | Palpitations or a sense of a pounding heart |
| Dizziness | Feeling lightheaded or unsteady |
| Hunger | A strong desire to eat, sometimes an “empty” stomach feeling |
| Anxiety | Feelings of nervousness or unease |
| Blurred vision | Temporary change in visual clarity |
How Neuropathy Alters These Symptoms:
- Reduced or absent adrenergic response: Those with neuropathy, especially autonomic neuropathy, might not feel the typical symptoms like shakiness, sweating, and rapid heartbeat because nerve signals don't trigger the release of adrenaline as effectively.
- Neurological changes: Instead of the usual physical symptoms, individuals might experience primarily neurological symptoms, such as confusion, difficulty concentrating, speech difficulties, changes in behavior, or extreme fatigue. These subtle shifts can easily be misattributed to other things, like tiredness or stress.
Specific Symptoms that Can Appear Due to Neuropathy:
- Mental Confusion: Difficulty with memory, disorientation, and trouble with thinking clearly are common.
- Fatigue and Lethargy: A sudden or severe feeling of tiredness and lack of energy that seems out of proportion.
- Speech Impairment: Difficulty articulating or slurred speech that wasn’t there before.
- Unusual Behavior: This may manifest as irritability, emotional changes, or behavior that is out of character.
The loss of classic symptoms such as shaking and sweating can cause significant delay in recognising an hypoglycaemic episode in people who suffer from diabetic neuropathy. Recognizing these less obvious changes becomes paramount in the safe management of diabetes in individuals with existing nerve damage.
The Importance of Routine Blood Glucose Monitoring and Proactive Management
Given the complexities introduced by neuropathy, especially the alteration of symptoms of hypoglycemia, continuous glucose monitoring and proactive management strategies are crucial. Routine blood glucose monitoring, particularly with continuous glucose monitors (CGMs), becomes invaluable. A CGM provides a constant stream of data, offering not only real-time readings, but also alerting the user if blood sugar levels are dropping too low, and provides data to demonstrate historical patterns that may not have been otherwise obvious. Here’s why this level of management is necessary and what it involves:
Importance of Routine Blood Glucose Monitoring:
- Early Detection: Regularly checking blood glucose levels helps in catching drops early when interventions are easier and more effective. Self-monitoring of blood glucose levels, either by capillary testing or a CGM should be a vital part of the routine, several times per day.
- Pattern Recognition: Monitoring over time reveals patterns, making it easier to understand how meals, physical activity, and medications impact blood sugar. For example, the user may find that they may be more vulnerable to hypos, at specific times of the day, allowing them to pre-empt issues.
- Dosage Adjustment: The results enable necessary adjustments to medication dosages under medical guidance, optimizing blood sugar levels without triggering lows.
- CGM Benefits: CGMs not only provide continuous readings but also alert users to impending hypoglycemia, which is extremely beneficial, particularly for individuals who may not experience the standard warning symptoms of a "hypo". Some more advanced systems, particularly those connected to insulin pumps, can automatically adjust or even stop insulin delivery, providing a critical safety feature for users with a high risk of nocturnal hypos.
Proactive Strategies for Managing Hypoglycemia Risk:
-
Personalized Diabetes Management Plan:
- Work with your healthcare team to create an individualized treatment plan which accounts for existing neuropathy.
- Adjust the timing and dosage of insulin or other medications to minimize hypo risks.
- Develop a structured eating plan with balanced, regular meals and snacks to prevent extreme blood glucose fluctuations.
-
Regular and Structured Eating:
- Do not skip meals, especially when you have been prescribed blood sugar-lowering medication.
- Make sure to have snacks available, when necessary, to prevent a fall in your blood glucose levels.
- Focus on a balanced dietary intake of complex carbohydrates, proteins, and healthy fats.
-
Physical Activity Precautions:
- Test your blood glucose levels before, during (if necessary), and after exercising, as physical activity will usually lower your blood glucose.
- Consume a snack as appropriate before prolonged physical activity to mitigate a potential "hypo" event.
-
Educate Friends and Family:
- Ensure that family, friends, or close acquaintances, understand the symptoms of hypoglycemia and what to do in an emergency.
-
Carry a Source of Quick-Acting Glucose:
- Always have a fast-acting source of glucose, such as glucose tablets or a sugary drink on hand for treatment.
-
Regular Healthcare Check-ups:
- Routine medical appointments allow for medication adjustment as required and management of both diabetes and any nerve damage issues. This includes annual reviews and neurological assessments.
When and How to Treat Hypoglycemia Effectively
Prompt and proper treatment of hypoglycemia is crucial to prevent severe complications, such as seizures and unconsciousness, especially when symptoms are masked by neuropathy. Knowing how to act swiftly and correctly can significantly impact patient safety. Here's a practical guide on when and how to treat low blood sugar effectively. The main treatment goal is to rapidly increase glucose levels.
When to Treat Hypoglycemia:
- Confirmed Low Blood Sugar: Any confirmed blood glucose reading below 70 mg/dL (3.9 mmol/L) requires immediate intervention. While the target range for most people is typically between 70 and 180mg/dL, healthcare providers should advise on individual targets that may vary based on specific needs and co-morbidities.
- Suspected Hypoglycemia: Even if you haven't checked your blood sugar but are experiencing symptoms suggestive of low blood sugar, especially if you have a history of hypos, you should proceed to treat as if your blood sugar were low, as it may be. Always follow your healthcare provider's advice.
- Nighttime Symptoms: Be especially alert to possible symptoms of hypoglycemia during the night. In some individuals, especially when they have neuropathy and hypoglycemia unawareness, the classic signs may be absent and this should be discussed with healthcare providers to ensure safe management. This includes symptoms such as restless sleep, night terrors, or unusually soaked night clothes.
Steps for Treating Hypoglycemia:
- Check Blood Glucose Levels: If possible, measure your blood sugar levels immediately to verify a "hypo" (but do not delay treatment if testing is unavailable).
- Consume Quick-Acting Carbohydrates:
- Take 15-20 grams of fast-acting carbohydrates, such as glucose tablets or gel, fruit juice, or regular soda, ensuring that any drink used is not a sugar-free version.
- Avoid foods that also contain fats as these can delay sugar absorption into the bloodstream and therefore, treatment may be less effective. For example, avoid eating chocolates.
- Wait 15 Minutes:
- After taking quick-acting carbohydrates, wait 15 minutes.
- Recheck Blood Glucose Levels:
- If after 15 minutes, blood sugar is still below 70 mg/dL (3.9 mmol/L), eat another 15-20 grams of fast-acting carbs.
- Follow Up with Longer Acting Food:
- Once your blood sugar reaches 70mg/dl (3.9 mmol/L) or higher, eat a snack with protein and carbohydrates, such as a sandwich, or fruit and nuts, to stabilize blood sugar and prevent it from dropping again.
- Contact Your Healthcare Provider: It's critical that your healthcare provider is aware of the "hypo" and any adjustments to treatment, as appropriate.
- Severe Hypoglycemia Treatment:
- Glucagon Kit: For severe cases, when a person has lost consciousness or is unable to swallow, a glucagon injection is essential. Glucagon can raise the blood sugar when a person has been unable to treat themselves using oral treatment. Caregivers or loved ones should be trained in the use of glucagon and ensure its availability at all times. After a glucagon injection, contact emergency medical services immediately.
- Emergency Medical Services: Call 911 (or your local emergency number) if the person has seizures, has passed out and cannot be roused, or if glucagon is not available.
The Long-Term Focus on Control
Ultimately, the goal is to minimize or prevent episodes of low blood sugar through a comprehensive and proactive approach to managing blood glucose levels. Effective communication with healthcare providers, self-awareness, and diligent monitoring are essential for patients suffering from diabetic neuropathy who are at a high risk of hypoglycemia, especially if symptoms are altered or absent. By consistently employing these strategies, those with neuropathy can significantly lower their risk of severe hypoglycemic events and maintain a higher quality of life. It's not just about responding to emergencies, but about proactively building a life where they are minimized.
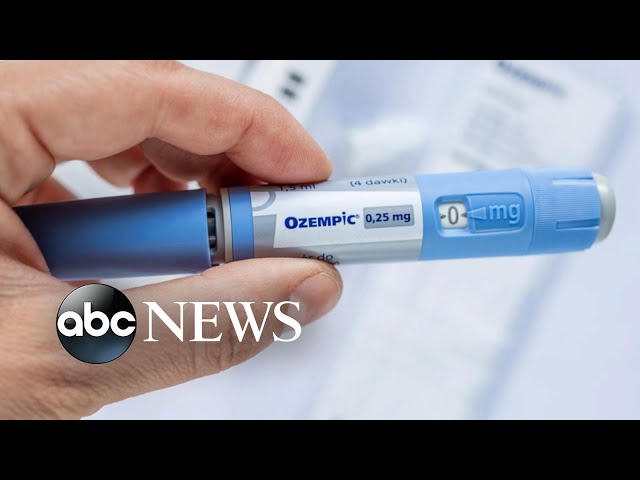
ABC News’ Stephanie Ramos reports on the sudden demand for a class of drugs approved for Type 2 diabetics but often used off-label to dramatically lose weight. ABC blood sugar miami News Live Prime, Weekdays at 7EST & 9EST WATCH exercises to reduce blood sugar levels the ABC News Live Stream Here: SUBSCRIBE to ABC NEWS: Watch More on can gluten raise blood sugar LIKE ABC News on FACEBOOK FOLLOW ABC News on TWITTER: #diabetes #drugs #weightloss